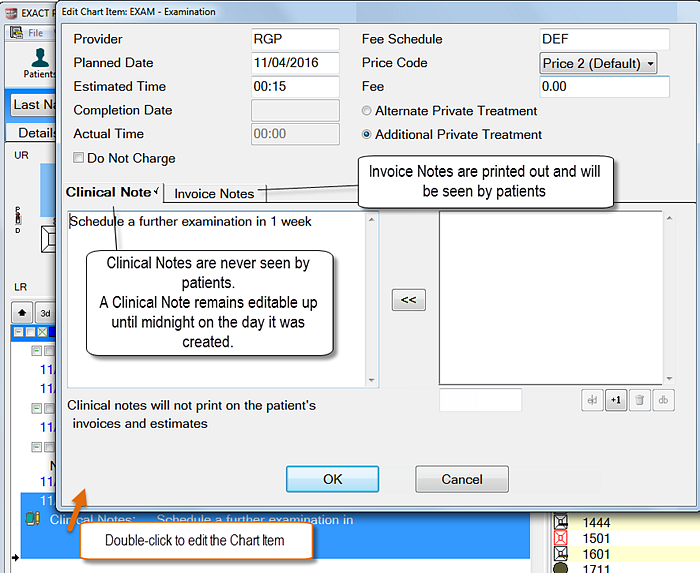
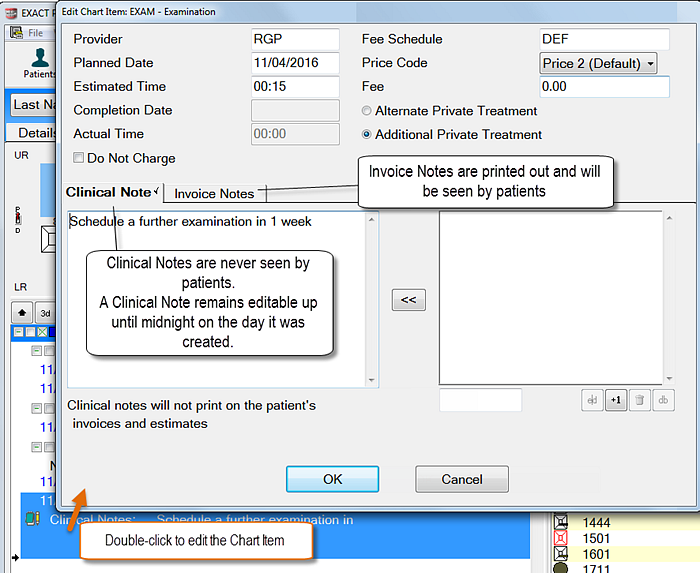
Charted Treatment can hold both Clinical and Invoice notes. You can also use the Note button to add general treatment notes that are not specific to a charted service.
Clinical Notes / Custom Screens remain editable up until midnight of the day they were charged or TC’d, after which they become read-only. This enables clinicians to process patients through the practice workflow and later write up important clinical note details. If a service is not ticked or ticked but not Charged/TC’d then the notes will remain editable until Charged/TC’d.
...
Entering Clinical or Invoice
...
Notes to a charted service
Clinical Notes are intended for use within the clinic and are seen by practitioners only.
Invoice Notes print on patients Statements, Estimates, & Invoices
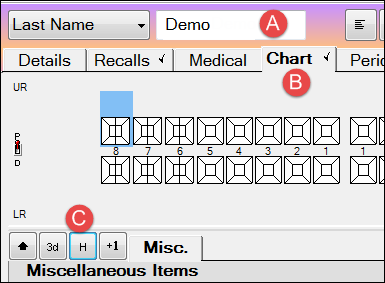
In a patient's chart tab, Double-click on the service in the Course of Treatment / Treatment Planning area
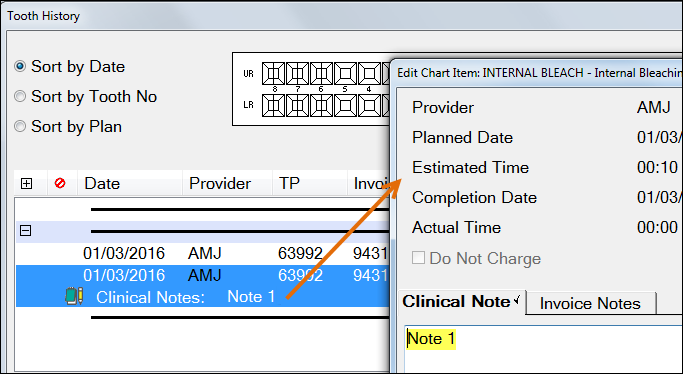
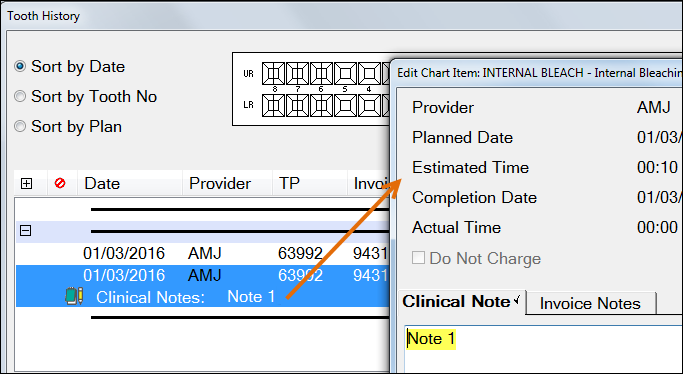
An Edit screen displays:
Type or use Quick Notes in the relevant tab and then click on the OK button to save.
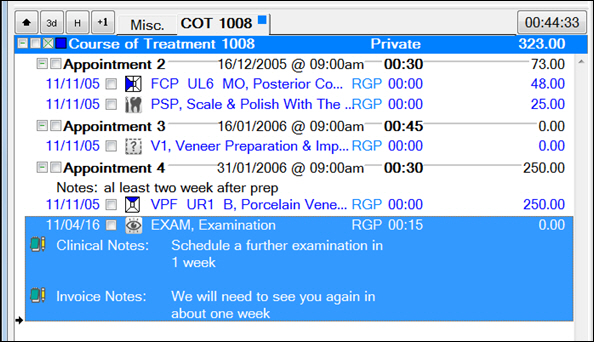
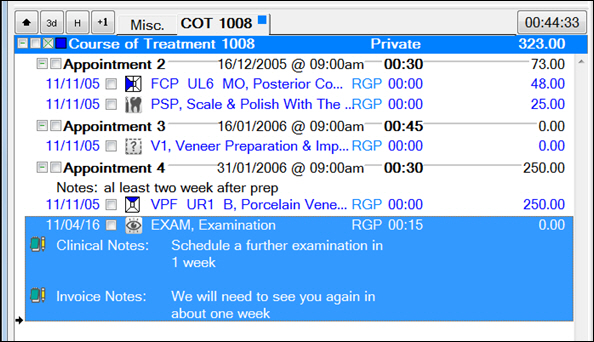
These notes display in the Chart tab.
Notes can also be viewed in the Tooth (Treatment) History tab. “H” button
Adding General Clinical Notes
...
using the Note Button
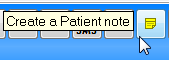
In addition to Clinical notes, which must be attached to a Service, the “Note” button at the bottom of the Treatment area provides the ability to create a General Note.
...
This is useful for recording notes when attending a patient but not actually providing any chargeable treatment, e.g., a review appointment.
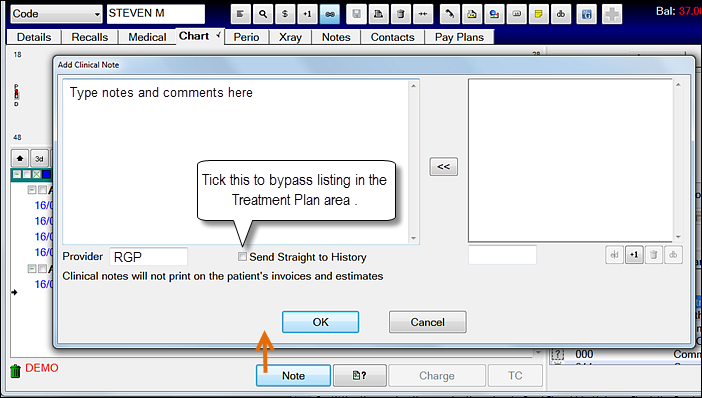
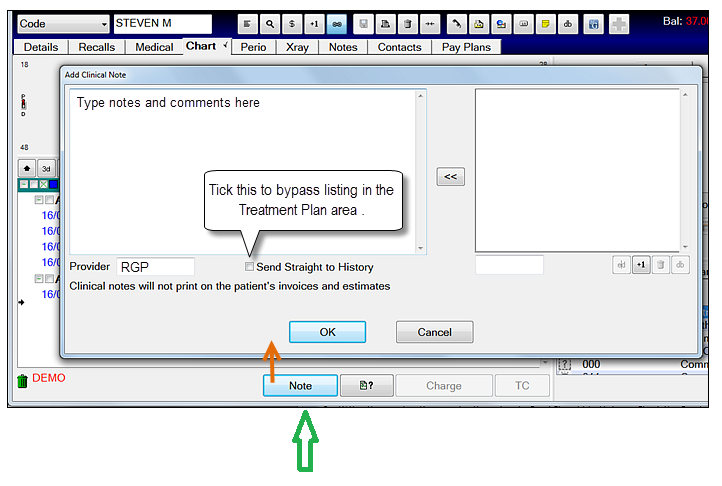
Click the Note button at the bottom of the Charting window to open the Add Clinical Note window:
Type or use Quick Notes as required. Specify the Provider if this hasn’t auto-filled.
Send Straight to History - Tick this checkbox to send this note directly into the patient's Treatment History window so it doesn’t appear in the COT. Leave it un-ticked to list it in the Treatment Plan area below the chart.
Click OK. Depending on the status of the checkbox, the Note will either list in the Treatment Plan area or in the History List.
Adding Appointment Notes
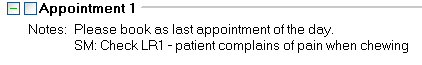
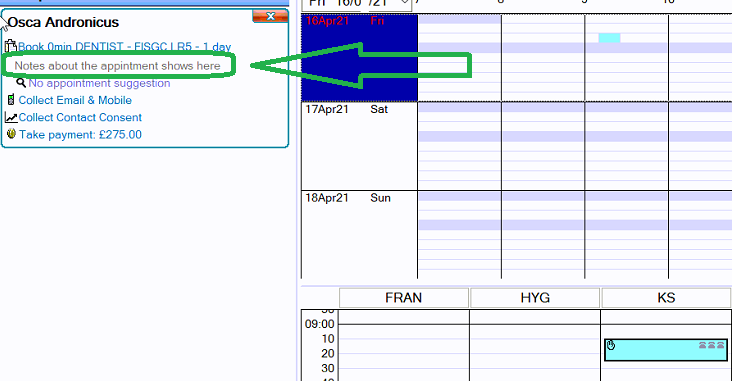
Often when an appointment is being created in the surgery a message may need to be sent to the receptionist regarding the appointment. These messages will be visible in the Appointment Book and in the Edit Appointment screen, which the receptionist will use to book further appointments.
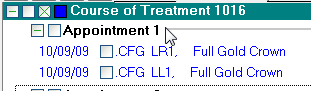
Double-click on the appointment in the Treatment Area. This is displayed on the Appointment line in bold black text:
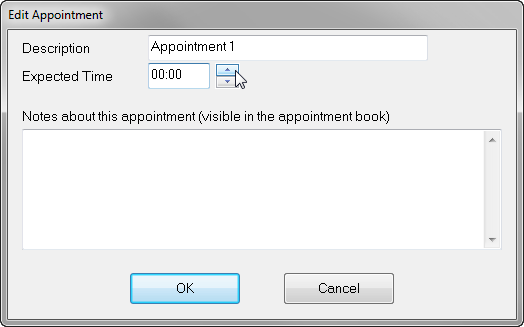
An Edit Appointment window will open:
Type any text in the Notes about this appointment… section and click on the OK button.
The notes will be visible at Reception and also attached to the particular appointment within the Treatment plan as well as the Depart bar for receptionists, as shown below:An alternative to this method of communicating with reception / providers is to use Pop up notes, which you create by clicking on the Notes button on the Toolbar:
Editing and Viewing Clinical Notes and Custom Screens
Historically, clinical notes and custom screens could not be edited once treatment was charged/invoiced.
This proved a bottleneck to practice workflow.
Receptionists were unable to process patients through departure and were unable to take payments if the Clinician's clinical notes and custom screens were unfinished.
Clinicians now have up until midnight of the day of treatment charging/invoicing to finalise the clinical notes and custom screens.
If treatment is resubmitted on a later day and then recharged, the clinical notes and custom screens remain editable until midnight of that same day (so the same procedure applies to new or resubmitted treatment that is charged).
EXACT Clinical Notes / Custom Screens remain editable up until midnight of the day they were charged or TC’d. EXACT maintains an un-editable audit trail of all clinical note and custom screen creation and editing in the Tooth (Treatment) History tab. Note that Previous Notes/Voided items in the audit trail are only visible when you check the Show Void checkbox in the Treatment History window:
...
...
You can optionally disable this capability for specific user groups.
Under Configure > Security, for a specified user group,open the permissions tree as follows:
File > Patients > Chart Tab > [ ] Allow Clinical Notes Editing on Charged Treatment
This permission is enabled by default, but you can un-check the checkbox to disable editing (remember to Save).
To edit Clinical Notes
...
& Custom Screens
Launch Double click the service on the COT tab on the Chart.
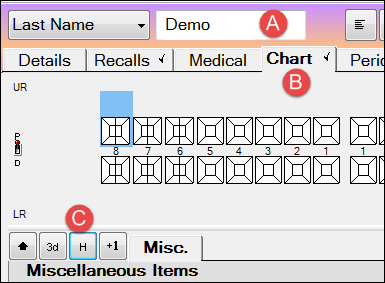
If the treatment has been sent to History or TC’d then launch the Tooth (Treatment) History window for a patient as follows:Select the Patient
Select the Chart Tab
Select the [ H ] History button
using the “H” button:
In the Tooth History window,
:
Locate and double-click the Clinical Note or Custom Screen, then edit itLocate and double-click the Custom Screen, then edit it:
Click OK.
To view edited Clinical Notes and Custom Screens
When you edit / change clinical notes and custom screens from the Tooth (Treatment) History, EXACT voids them and displays only the latest version.
Check the Show Void checkbox to see all "voided" (changed) items.
Example (Clinical Note):
Here is the original:
...
This was edited from the Treatment History and then saved:
...
Check the Show Void checkbox to see the voided (changed) notes:
...
as required and click OK to save.